Hi students, here is an example of a real life case that is handled by a pathologist in the diagnostic pathology laboratory.
This is a COLONIC TUMOUR from a right hemicolectomy specimen that is received from the operating theatre.
The pathologist’s role is to provide diagnostic and prognostic information for the managing team (surgeons, medical and radiation oncologists etc).
For every case the pathologist receives, he or she will:
- Examine the specimen grossly (in this case, identify the tumour, lymph nodes, etc.)
- Trim the specimen – sample specific areas for microscopic examination
- Examine the specimen microscopically to evaluate prognostic factors
- Reporting – prepare a Pathology report for the managing team
Let’s walk through this case from the beginning:
I. History and relevant investigations
Mr Tan, a 77 year old retired taxi driver, presents with lower abdominal pain and loss of weight over the past 3 months. He had a faecal occult blood test which was negative.
(Click HERE to find out more about faecal occult blood test as a screening tool for colorectal cancer in Singapore.)
Colonoscopy was performed:
Colonoscopy showed an annular tumour in the distal transverse colon causing luminal constriction. The endoscopist was unable to pass the endoscope beyond the tumour. A biopsy was taken and Mr Tan was diagnosed with colorectal adenocarcinoma.
Other findings include a polyp distal to the tumour. Biopsy revealed a tubular adenoma.
Staging investigations included CT scan of the thorax, abdomen and pelvis which showed no other tumour deposits.
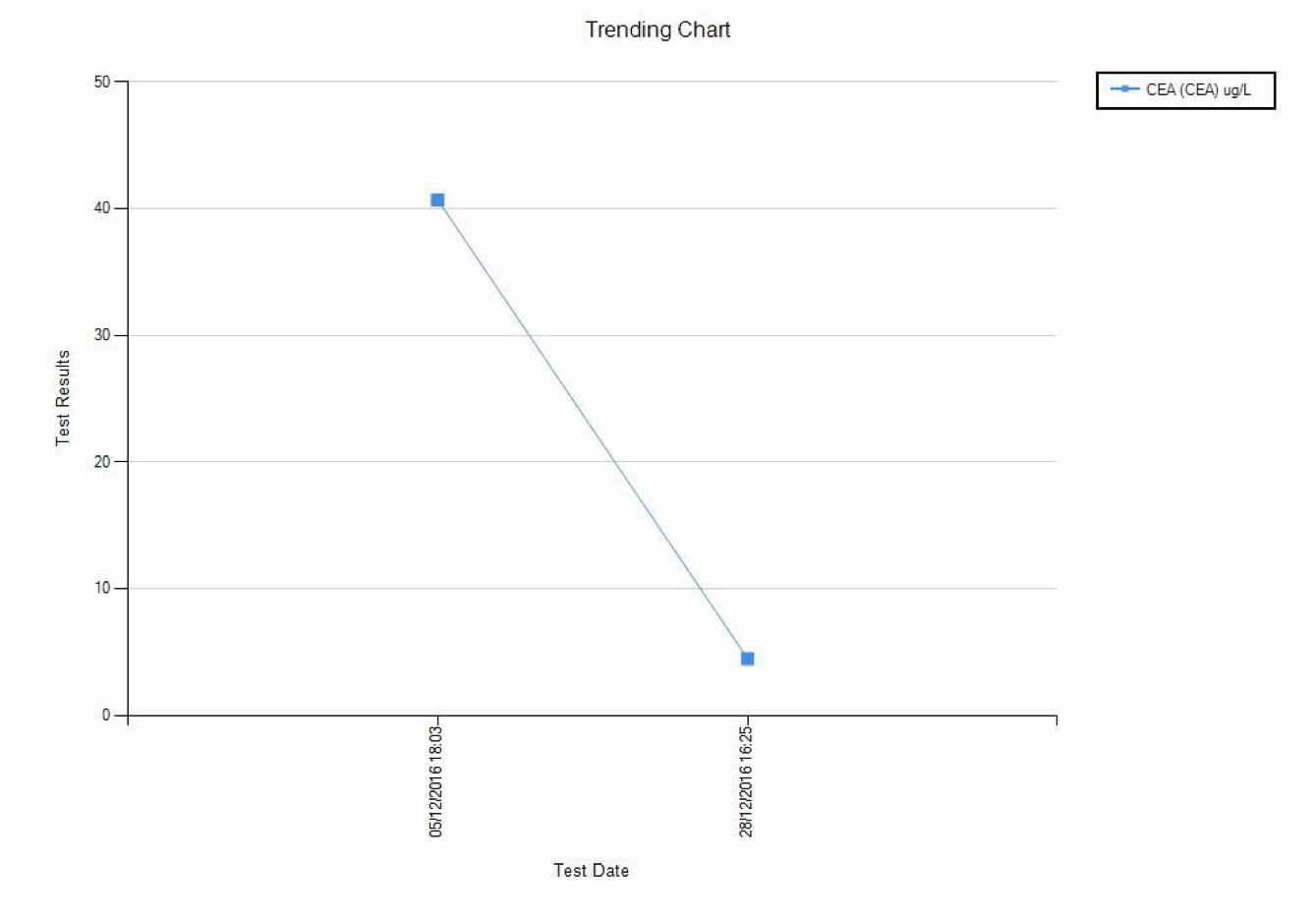
His baseline serum CEA was 41ug/L. CEA is a tumour marker for colorectal cancer and can be used to monitor response to therapy and disease recurrence.
Mr Tan underwent an extended right hemicolectomy and the specimen was sent to the pathology lab.
II. In the Pathology Lab
Upon receiving the specimen, the first step is to describe it and sample relevant tissues for microscopic examination. This is called “Grossing”.
Video 1. Grossing the colon
The sampled sections and then processed into sections on glass slides.The pathologist examines them.
Video 2: Microscopic examination
III. Final Pathology Report
The pathologist then writes a report of his/her findings, which is conveyed to the managing team.
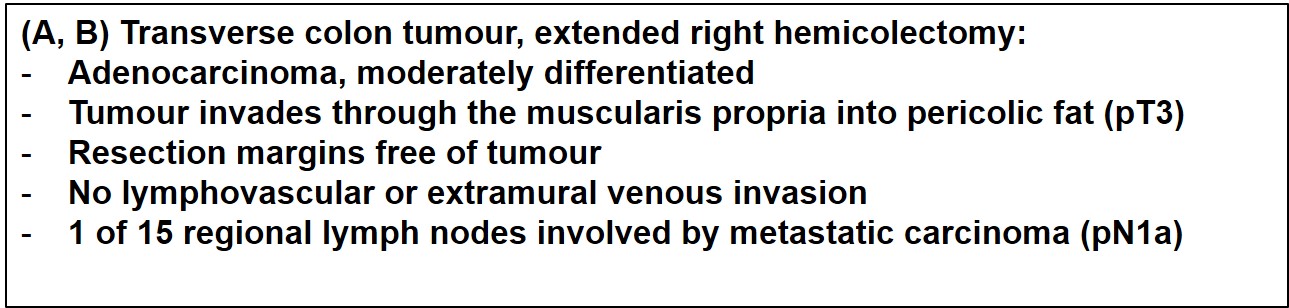
According to the TNM staging for colorectal cancer, pT3 N1a M0 belongs to the cancer stage group IIIB. The prefix “p” represents pathological staging (on microscopic examination).
IV. Post-operative care and beyond
Mr Tan had an uncomplicated post-operative recovery and was discharged from hospital 6 days after the surgery.
His case was discussed at a multi-disciplinary team meeting (Colorectal Oncology Tumour Group). This is a weekly meeting attended by surgeons, oncologists, pathologists, radiologists, nurse consultants and allied health professionals involved in the care of patients with colorectal cancer.
The consensus was that Mr Tan should have post-operative chemotherapy, as it has been shown in clinical trials to offer survival benefit in patients with a similar stage of cancer.
Mr Tan was seen at the oncology outpatient clinic 1 month after the operation, where he decided not to have chemotherapy. He will have follow-up CT scans and his serum CEA level will be monitored according to local protocols.
Carcinoembryonic antigen (CEA) is a glycoprotein normally found in epithelium of endodermal origin. It may be raised in the serum of patients with primary colorectal cancer or other malignancies including medullary thyroid carcinoma and breast, gastrointestinal tract, liver, lung, ovarian, pancreatic, and prostatic cancers. It may also be raised in smokers. Current uses of serum CEA include measuring response to treatment and monitoring disease recurrence.
Post-operatively, Mr Tan's serum CEA level decreased significantly. Hence, it has shown to be a useful marker in monitoring tumour burden in Mr Tan.
Limitations
- Poor diagnostic efficacy
- Serum CEA should not be used to screen asymptomatic individuals for neoplastic disease, as diagnostic efficacy in high-risk groups has not been established
- Serum CEA should be used in conjunction with information from the clinical evaluation of the patient and other diagnostic procedures
- Not all colonic tumours result in raised serum CEA. Therefore, monitoring post-treatment CEA levels is only useful in cases which have initial raised CEA, like Mr Tan.
- CEA values are method-dependent; therefore, the same laboratory method should be used to serially monitor patients
This case demonstration was jointly created by Dr Seet Ju Ee, and Noel Chia (University of New South Wales, Class of 2017).