When the autonomic nervous system ganglia are activated (for example, by low-dose nicotine), both the sympathetic and parasympathetic nervous system innervations of target organs and tissues are simultaneously stimulated. However, the “fright, fight or flight” sympathetic and “rest and digest” parasympathetic nervous systems have opposing effects in most target organs and tissues. So why do the sympathetic and parasympathetic nervous systems not just cancel each other out when activated at the same time?
It is true that in the realm of autonomic nervous system functioning, the sympathetic and parasympathetic systems often represent two sides of the same coin. These systems largely produce opposing effects on the same target organs and tissues. However, what happens when both systems are simultaneously activated? Contrary to intuitive thinking, they don’t simply cancel each other out. Instead, the dominion of activation or excitatory effects takes centre stage.
The Principle of Dominant Excitation: When both the sympathetic and parasympathetic systems are co-activated, it isn’t a zero-sum game. Rather than neutralizing each other, the excitatory effects from each system generally prevail. This principle is observed in a variety of physiological contexts. Continue reading
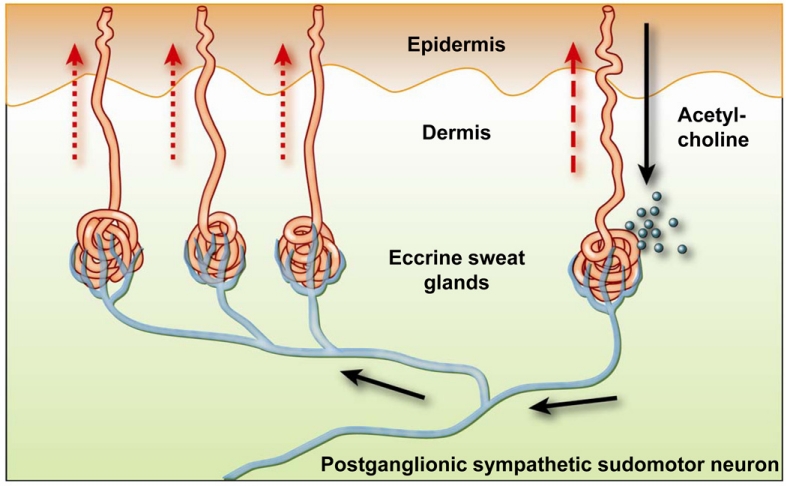 Image credit:
Image credit: